Dancing with the Enemy
The malaria parasite’s life cycle relies on humans and mosquitoes. Could we use the mosquito to stop the parasite?
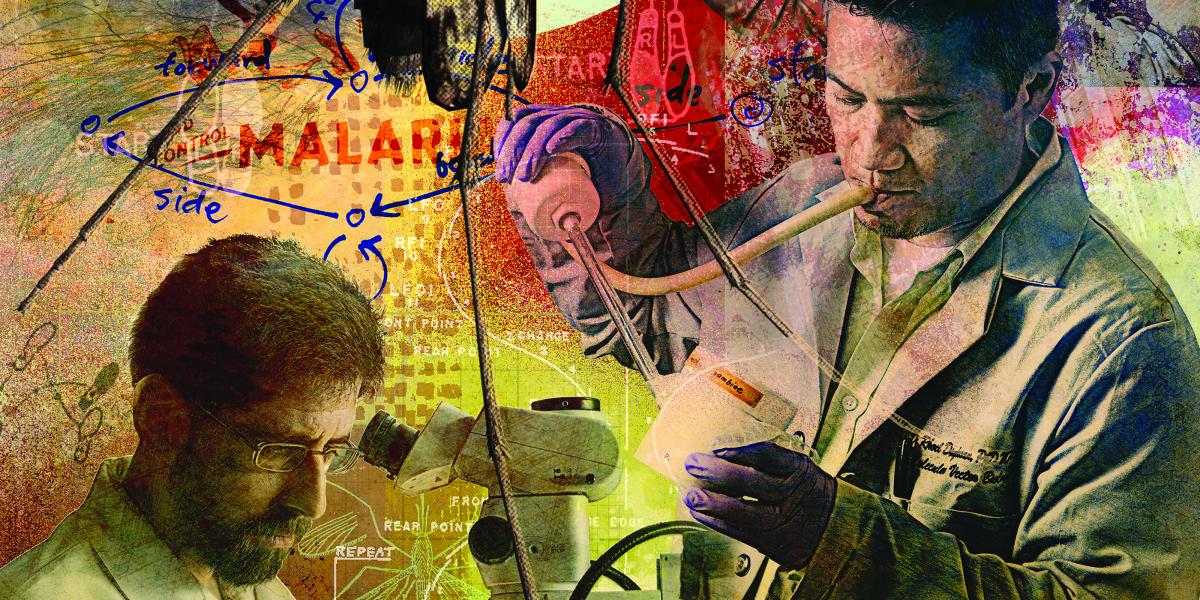
The small sign on the door designating the space as the Johns Hopkins Malaria Research Institute’s Core Insect Facility doesn’t do justice to the utter creepiness of what lies waiting inside. Carved into the sterile white walls are doors marked with the names of mosquito species: A. stephensi, A. gambiae, A. funestus. Within these rooms is a disconcerting nursery.
Tiny, tadpole-like larvae float in water in plastic bins on shelves. They are sustained by a single, bloated cat-food pellet. The bins holding older pupa are topped with a layer of mesh held down with lead weights, anticipating their transformation into flying and biting adults. A grad student stands in the corner with an adult-filled bin. Carefully, he uses a vacuum hose to transfer the bugs into mesh-sided cubes, where a dense array of mosquitoes line the walls and buzz around inside. A bug zapper near the ceiling shines blue light—ever ready to catch any escapees.
As an anxious visitor to the A. stephensi room, I rub my bare arms and wish I’d worn long sleeves. Warily eyeing the bug-filled boxes, I tell insectarium director Marcelo Jacobs-Lorena, PhD, MS, Molecular Microbiology and Immunology (MMI) professor, that the room’s hundreds of mosquitoes are really disturbing. “That’s okay,” he laughs. “If you feel that way, then it gives you even more pleasure to dissect them.”
It’s the fate that awaits many of these Anopheles mosquitoes. That’s because these insects are one of JHMRI’s greatest resources in the fight against the disease. The bugs host the malaria parasite, Plasmodium. That makes mosquitoes an obvious target for efforts to stop malaria.
Several researchers at JHMRI are concentrating on this very goal, focusing on various ways to use the mosquito to block transmission: either by decreasing mosquitoes’ own defenses against Plasmodium, shortening their life span so they die before passing on the disease, or developing an innovative vaccine for people that blocks Plasmodium infection in mosquitoes. To solve malaria, they say, we have to partner with the very vector responsible for transmitting the disease.
The Clues Genes Hold
As I lean back in a comfortable chair in Jacobs-Lorena’s office, warmed by late afternoon sun and safely distant from any six-legged intruders, he explains in a musical accent that reveals his Brazilian heritage that targeting the mosquito is far from a novel idea. As soon as people realized that malaria sprouted from the proboscis of this tiny insect, scientists have been working on strategies to kill off mosquitoes or minimize contact with these bugs to prevent bites. The two most effective strategies for preventing malaria thus far have been widespread use of insecticides and bed nets (both plain and treated with insecticides).
However, these approaches have drawbacks. Heavy use of insecticides, most notably DDT, has led to whole populations of mosquitoes that are resistant to these poisons. Insecticides also aren’t the most eco-friendly of interventions, and they require constant follow-up—often unsustainable in poor locales. Bed nets—which are easily ripped and wear out over time—are also far from perfect.
Consequently, scientists will need to find new ways to interact with the other half of malaria’s host dyad to slow or prevent infection rates. But before we form a close relationship with an arthropod, it will be crucial to know exactly who we’re working with, says Douglas Norris, PhD, MS, MMI associate professor.
In many places in which scientists would like to target mosquitoes, they’re still pondering lots of basic questions: Which species are actually present in a region? Do they bite just humans, or do they take their meals primarily from other animals? If humans are their food source of choice, are they biting many people sequentially, or do they get a full meal from just one at a time? How many of these human blood suckers are infected with Plasmodium and currently infectious?
To address such questions, Norris and his colleagues are going straight to the insect source, using high-tech genetic methods to derive answers. They have partnered with colleagues in Macha, Zambia, and elsewhere to gather mosquitoes for study. These collaborators ensnare mosquitoes using a variety of methods—one of the most popular is installing a light trap right above a sleeping human, who’s safely covered with a bed net—then freeze them for later study.
Potentially important species are identified through a number of steps, first of which is visual inspection under the microscope. Then, the scientists pop off the insects’ head and thorax (which have salivary glands that contain infectious Plasmodium parasites) and their abdomens (which may contain blood if a mosquito has recently fed) and place them in a small tube with a dollop of silica gel and a cotton plug. Norris explains the procedure as he hands me a tiny plastic tube rattling with dried insect pieces mummified by the silica gel.
When the researchers are ready, they can run a variety of tests on the heads and thoraxes. Since many mosquito species and subpopulations look alike, researchers can examine the mosquito’s own genetics to determine exactly which one is in the tube. Such knowledge aids efforts to create and disseminate genetically altered mosquitoes—which requires transformed lab mosquitoes carrying the “anti-Plasmodium” genes to breed with existing populations.
“Researchers working on genetically altered mosquitoes are operating on the assumption that the target population for each species is one big, happy breeding population. But what if, instead, this group is structured into subpopulations that don’t breed with each other?” Norris asks. For example, he says, work with his collaborators at the University of California-Davis has shown that a population of Anopheles arabiensis in central Africa is separated into groups that don’t interbreed. “If the subpopulations don’t interact, then you’ll only get your new gene into one population. That one subpopulation will be converted, but you’ll still potentially have malaria transmission by the other populations—if they’re not interbreeding or the gene isn’t introduced to each population, your whole strategy may fail.”
Understanding if mosquito populations are interbreeding can also tell you whether or how speedily they could be swapping genes, Norris adds. That’s particularly important for strategizing against insecticide resistance, a trait that mosquitoes can acquire through random genetic mutations. If mosquito subgroups are heavily interbreeding, then it’s practically a given that the mutation for insecticide resistance will sweep through the population quickly. However, if the subgroups are giving each other the cold shoulder, then researchers may have more time to develop an action plan to control insecticide resistance.
The desiccated insect body parts can yield answers to other basic questions as well. Any blood that remains in a mosquito’s abdomen from a recent meal can tell researchers which animal it’s recently fed on. If it’s human, Norris’ group can also search deeper to see if multiple people’s blood is present in the same insect. Moreover, they can look for Plasmodium genes or antigens in the mosquito’s salivary glands, a dead giveaway that the insect was infectious at the time of its death.
Gaining such genetic information has already proved useful, Norris says. In a recent study, he and his colleagues examined human blood isolated from mosquitoes caught in Macha to see whether it came from male or female victims. Sex markers in the blood showed that women were bitten most often—perhaps because they get up earlier and go to bed later than men in this particular area, leaving them vulnerable during mosquitoes’ prime biting hours. This information could help researchers target an education plan to encourage women and others to protect themselves from mosquitoes if they’re awake while the insects are active.
Building "Super Immunity"
Protecting humans from malaria is the obvious goal here. But, says George Dimopoulos, PhD, MBA, protecting mosquitoes from malaria accomplishes the same goal. If researchers could successfully create a mosquito that is immune to Plasmodium, then these insects would be unable to continue the parasite's life cycle and pass it back to humans.
One way to shield mosquitoes from Plasmodium is to bump up the power of their own immune systems. Any normal, healthy mosquito already has the capability to kill off the parasite once it gets infected, explains Dimopoulos, MMI associate professor. "Susceptible mosquitoes that get Plasmodium activate their immune system and kill off large numbers of parasites, but a small number [of parasites] make it through," he says. That small number eventually becomes the population that gives people malaria.
If only researchers could make mosquitoes' immune systems stronger and more resistant to Plasmodium, then the insects could kill off all the invading parasites and have complete immunity. Making these super-immune mosquitoes is a major focus for Dimopoulos and his lab.
Last year, he and his colleagues discovered a network of genes that are part of the immune deficiency (IMD) pathway and allow mosquitoes to fight off Plasmodium. This pathway (so-named for the fly in which it was discovered, which had an immune deficiency) controls a protein called Rel2. When the parasite-fighting IMD pathway is turned on, Rel2 binds to a mosquito's DNA and activates production of parasite-killing molecules. Experiments show that's what seems to happen during a natural malaria infection—albeit too late and too weak to catch all the parasites before an infection takes hold. This pathway doesn't stay running all the time, explains Dimopoulos, since it would take too much of a mosquito's resources to maintain.
He and his team also discovered Rel2's shutoff valve, a gene called caspar, which they manipulated to show that strong activation of the IMD pathway can give mosquitoes Plasmodium resistance. Knowing the components that go into running the IMD pathway allowed them to use genetic engineering to construct an elaborate system in which they linked Rel2 to the gene for a digestive enzyme. That means that once mosquitoes take a blood meal and get to work on digesting it, Rel2 is activated, which jump-starts the malaria-fighting pathway. "Once the parasite tries to infect the mosquito, it will encounter a very hostile environment," Dimopoulos explains.
He and his colleagues are currently studying the genetically engineered strain of mosquitoes they created with this modification to better understand exactly where, when and how Plasmodium is killed and to see whether they can optimize this process. In the meantime, they're also examining a different system that mosquitoes use to fight off malaria: their gut bacteria. "Mosquitoes have a significant population of symbiotic microbes in their intestine that play an important role in fighting off infectious invaders. Humans also have an intestinal 'microbiome,'" which fulfills the same function, explains Dimopoulos.
Dimopoulos' lab has painstakingly searched through the various species that inhabit mosquitoes' guts to see if any has especially good Plasmodium-fighting power. They recently discovered one that seems to possess significantly more parasite-inhibiting power than the others. They are currently delving into how this microbe species battles Plasmodium, efforts that could lead to using this bacterium, or the strategy it employs against the parasite, as a key warrior in the fight against malaria.
Gut-Level Investigations
Jacobs-Lorena and MMI assistant professor Jason Rasgon, PhD, are also hoping to capitalize on mosquitoes' gut bacteria, though in completely different ways.
Jacobs-Lorena led one of the first teams working to genetically modify mosquitoes to make them resistant to malaria. He's since switched tactics, focusing now on genetically modifying the gut bacteria instead. This strategy might solve one of the most puzzling problems of genetic modification in general: how to get the desired gene into the target population. Rather than taking a roll of the dice on mosquitoes' somewhat puzzling sex lives, Jacobs-Lorena notes that getting the target genes inside mosquitoes, packaged inside bacteria, could be a significantly easier exercise. Since all mosquitoes eat—and supplement their blood meals with carbohydrates—mixing some modified bacteria with sugar could be enough to do the trick. Some gut bacteria are passed on from mother to offspring, so starting the process with one generation could keep it going indefinitely.
His lab is currently working on perfecting the right mix of anti-Plasmodium genes in gut bacteria. It's important to have several genes that fight the parasite in different ways, he explains: "You can never rely only on one. Then you'd have the same problem that you'd have with antibiotics on bacteria that make people sick—with time, the parasite becomes resistant."
He and his team recently tested this approach in live mosquitoes from the insectaries he directs, infusing them with bacteria whose new genes produced a variety of malaria-combating proteins. For example, some block the parasite from passing into a mosquito's midgut through a mechanism the scientists still don't understand. Regardless, these useful bacteria reduced by 80 to 90 percent the formation of oocysts, pouches filled with the precursors of Plasmodium's motile form that eventually infects humans. The researchers are optimizing those numbers through further modifications.
Rasgon's work with bacteria aims to shorten the insects' life spans so that they don't live long enough to pass on the parasite. His main focus is a genus of bacteria known as Wolbachia. Researchers have long known that these microbes infect insects, with about 70 percent of species affected. More specifically, Wolbachiainfects nearly every genus of mosquito—that is, except for those in the genus Anopheles, the one that carries the malaria parasite.
Since a Wolbachia infection can significantly shorten an insect's life span—hastening death but not before the insect breeds, reducing the evolutionary pressure for an insect species to develop resistance—it would be a boon to develop a way to infect Anopheles. Though it takes some effort in the lab, getting the bacteria into the mosquitoes' cells or bodies is a doable feat. However, unlike other insect species, female Anophelesmosquitoes don't transfer Wolbachia to their offspring, making the process of sustaining the infection through successive generations impossible.
After nearly a decade of trying to make sustainable Wolbachia infection a reality for Anopheles, Rasgon is expecting success in a couple of years. "We've been at this a long time—it's become personal now," he says, with a look that combines both hardened determination and a murderous glint, presumably geared toward mosquitoes.
In the course of working on Wolbachia, Rasgon and his colleagues—by accident—found a virus living in a line of mosquito cells. In live mosquitoes, this virus, called AgDNV, doesn't appear to affect the insects in any way, but tests show that it peaks in reproduction right before the insects are old enough to pass on the malaria parasite. His lab is currently working on using the virus to express some kind of mosquito toxin that could work in a similar way to Wolbachia, by shortening the insects' life spans before they can infect people with malaria.
Toward a Transmission-Blocking Vaccine
In contrast, Rhoel Dinglasan, PhD, MMI assistant professor, has developed a unique strategy with an intervention that isn’t administered directly to mosquitoes. Instead, it targets mosquitoes indirectly through their food source: humans. He’s creating a new vaccine that imbues mosquitoes with malaria-fighting power through antibodies in human blood. One blood snack would lead to Plasmodium protection for the insects, as well as protection for the next person that a mosquito bites.
Dinglasan’s vaccine isn’t the only “transmission-blocking” vaccine in development. Several research groups, including one led by former JHMRI Professor Nirbhay Kumar, PhD, have worked on similar approaches for decades. However, Dinglasan’s methodology has quickly gained the backing of the malaria community, including the PATH Malaria Vaccine Initiative, which funds other promising malaria vaccine initiatives. The recent stir over Dinglasan’s work is due to its unique success in attacking the two most common human malaria parasite species in all the species of mosquitoes tested thus far.
While completing his PhD, Dinglasan had become interested in the various naturally occurring sugars that attach to proteins present throughout mosquitoes—sugar-coated proteins known as glycoproteins. At the time, little was known about these glycoproteins. However, previous research had shown that glycoproteins in the mosquito’s midgut in particular appear to play a key role in Plasmodium’s ability to invade mosquito cells and set up an infection.
Dinglasan hatched the idea as a postdoc in Jacobs-Lorena’s lab. There, he identified a key midgut glycoprotein called aminopeptidase 1 (APN1) that’s present in all mosquitoes. This protein is a digestive enzyme that’s always present in the mosquito midgut, ready to digest a blood meal as soon as the insect consumes one.
However, this protein also appears to play another role: It’s necessary for Plasmodium infection. Dinglasan and his colleagues found that when antibodies to a portion of this protein are present in an infectious blood meal, mosquitoes were 100 percent protected from the parasite.
To get these antibodies efficiently into mosquitoes, Dinglasan relied on the same strategy used by the creators of other transmission-blocking vaccines: creating antibodies in the people that mosquitoes bite. When mosquitoes take a blood meal, they pick up the antibodies.
So far, Dinglasan and his collaborators have produced the protein fragment that serves as an antigen that spurs people to make antibodies to the APN1 protein. In the next two years, they hope to test this vaccine in clinical trials. To eradicate a disease, Dinglasan says, its cycle of transmission must be broken—that strategy worked for smallpox.
“Malaria researchers have real opportunities to include new approaches to break the cycle of malaria transmission,” Dinglasan says. “We have to take them.”