The Double Jeopardy of Environmental Racism
Black Americans are more likely to live near pollution sources that set off a dangerous cascade of health problems.
Glenn Ross remembers the sunflowers in a field near where he grew up in Baltimore’s Fort Worthington neighborhood. His family and neighbors enjoyed the flowers’ beauty and the taste of the freshly picked seeds, sautéed in butter with a pinch of salt.
They didn’t know that the sunflowers, like the nearby African ferns, were in the former cemetery for phytoremediation—the use of plants to remove contaminants like lead and arsenic from soil, standing water, and air.
From the 1950s into the 1970s, Armco Inc., a steel processing plant, dumped hundreds of thousands of cubic feet of construction debris and processing waste there before burying it under a few inches of soil. The area is now a fenced-off landfill. Ross, a 70-year-old environmental advocate, stops at the site, covered with grass and shrubs, on his Urban Environmental Toxic Tour.
“That’s one of three landfills within the eight-block area of this neighborhood. This area here, of East Baltimore, has the highest respiratory and asthma problems in the whole city,” he says, adding that he attributes his health complications, particularly asthma, to a lifetime of being exposed to contaminants.
Ross’s experience is not unique. His concerns about the proximity of landfills, factories, and other pollution sources are echoed in Black communities across the U.S. A 2015 Environmental Research Letters study concluded that race is the largest risk factor for living near a hazardous waste disposal facility. Blacks and Hispanics are exposed to particulate matter—fine inhalable particles like dust and soot released by burning fossil fuels—at a rate more than 50% higher than whites. And a 2016 Reuters report found nearly 3,000 disproportionately poor and Black locations where blood lead levels were double those of Flint, Michigan (affected by a 2014 contaminated water crisis). Even middle-class Black Americans are exposed to significantly higher levels of pollution than whites with annual incomes of $10,000.
The evidence of environmental racism is clear, says Genee Smith, PhD, MSPH, an assistant professor in Environmental Health and Engineering. It follows from racist policies that disproportionately leave nonwhites with the “double jeopardy” of experiencing multiple environmental stressors that intensify existing health disparities.
“Environmental racism is systemic—it is rooted in the devaluing of nonwhite lives and the hoarding of wealth—and built into public policies,” says Smith. “Dismantling environmental racism requires transformational policies which provide both restoration to the land and redress to the people that have endured this form of violence.” She adds that land-use zoning policies and discriminatory housing practices intensify threats to Black Americans and other people of color.
Numerous “environmental insults”—exposures to hazardous wastes, contaminated water, and air pollution—have been slowly eroding the health of Black Americans, as well as other people of color and low-income individuals, for decades, says Aisha Dickerson, PhD, MSPH, a Bloomberg Assistant Professor of American Health who studies environmental exposure and the accompanying risk for neurological diseases. Higher levels of exposure among poor people and nonwhites are compounded by barriers to testing and health care, which leave them less likely to receive a diagnosis or treatment.
Dickerson compares these constant environmental insults to a wound without an opportunity to heal. The bodies of many Black Americans are fighting off too much, too continuously to recover.
Merely removing the lead or other toxins of concern is not enough, Dickerson says.
“Lead can store in bone over several decades. When someone ages and bone begins to degrade, [lead] can remobilize and leak into the blood. [While] your brain may not have been exposed to it in middle age, you could be re-exposed in older age,” she states. A similar reexposure can happen to women who were exposed to the toxin at a young age: lead stored in bone is remobilized when bone is metabolized during pregnancy and breastfeeding.
An environment of consistent toxic exposures can lead to cascading health problems. Everyday toxins like pesticides, mold, and mildew—which Dickerson notes are particularly common in public housing—can cause inflammation. Chronic inflammation raises one’s risk for complications ranging from weight gain to degenerative diseases like Alzheimer’s, autoimmune diseases, and diabetes. Simultaneously, continued environmental insults increase one’s risk for a myriad of cancers, respiratory and cardiovascular complications, and more recently, COVID-19.
Dickerson compares these constant environmental insults to a wound without an opportunity to heal. The bodies of many Black Americans are fighting off too much, too continuously to recover.
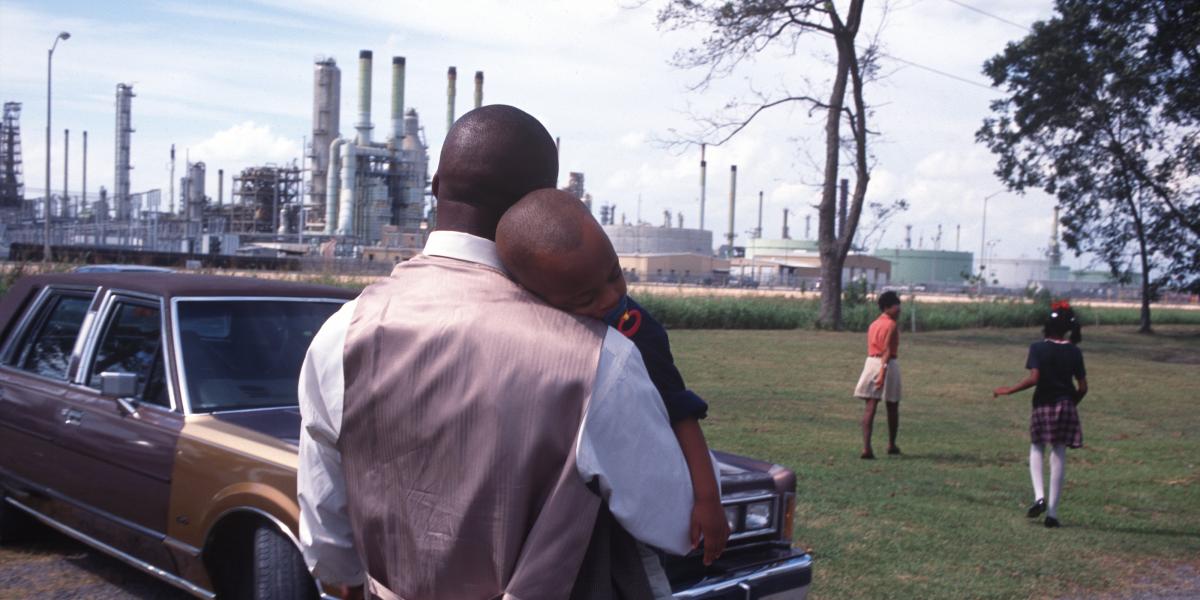
The real-life consequences of these environmental insults can be witnessed in places like Cancer Alley in Louisiana, an 85-mile stretch of the Mississippi River lined with oil refineries and petrochemical plants. In St. Gabriel—the town that first gave Cancer Alley its ominous nickname—toxic air levels from cancer-causing chemicals are higher than in 99% of the country, according to a 2019 ProPublica analysis. Like many towns along this industrial corridor, St. Gabriel is decidedly nonwhite: two-thirds of its residents are Black.
And Black communities that take on environmental racism are often thwarted. Residents of Uniontown, Alabama—nearly 90% Black with a median income of just over $14,000—fought back against a permit granted to operate a landfill less than a mile away. They lost a years-long legal battle after the EPA determined there was “insufficient evidence” that the landfill increased their health risks.
Cases like these demonstrate the complicated network of social, economic, and environmental factors that create health disparities for Black people, say Smith and Dickerson. They point to the legacy of discriminatory economic and housing policies, such as redlining, the use of subpar building materials, and zoning and building codes that allow companies to construct facilities that produce toxic wastes near communities of color.
Dickerson calls on public health researchers to do more than quantify the disparities.
“[If you’re not] educating people at the community level or trying to make some type of policy change, then you're not really doing your job," she says, adding that effective researchers work at the individual, community, and policy levels.
“Ultimately,” says Smith, “we must acknowledge that environmental equity cannot be achieved without racial equity.”