Acral Lentiginous Melanoma: The Overlooked Cancer
The most common melanoma among people of color is also one of the least researched. That is changing, finally.
When Suzanne Carothers left North Carolina for graduate school in New York City nearly 50 years ago, she carried with her a weighty book and three pieces of advice.
The book was the Physicians’ Desk Reference. The pieces of advice: Always do your own research, ask questions, and be an advocate for your health.
Her mother, a Black registered nurse, had often seen Black patients receive inadequate medical care at the hospital where she worked in Charlotte. She wanted her daughter to be informed and prepared.
Carothers heeded her mother’s advice. She saw a few moles on her body when she was in her 60s and began seeing a dermatologist. Then, at an annual screening last year, her dermatologist checked the soles of her feet and noticed a dark spot near her heel. It was acral lentiginous melanoma, a rare subtype of melanoma that appears on the palms, on soles of the feet, or under fingernails or toenails.
Carothers, now 71 and also a breast cancer survivor, was lucky: Her dermatologist had caught it early. After having surgeries to excise the cancerous cells and additional skin around the margins, she’s in remission. But the majority of ALM patients tend to present later, when the cancer is more difficult to treat. And Carothers now wonders why no one had ever checked for this before.
“I’ve been to all kinds of doctors,” she says. Until that visit, “no doctor has ever looked at the bottom of my foot.”
ALM is a strange cancer. While most cases of cutaneous melanoma in the U.S. are linked to UV radiation from sun exposure, ALM is not. It’s relatively rare, making up just 2%–3% of U.S. melanoma cases and about 2,000 cases overall. But it also may be the most common form of melanoma in many countries because it makes up 50% to 80% of melanoma cases among people of color. Studies in Mexico, Taiwan, and China, for example, have found ALM to be the most common melanoma subtype in their populations. Even so, it’s also one of the least-researched cancers.
Since there are no known means of preventing ALM, the best alternative is to spot it early. Here again, science and the health system have fallen short: Most of the people at greatest risk for ALM have never heard of it.
Tracey Liebman, MD, the NYU Langone Health dermatologist who treated Carothers, described one ALM patient who attributed the dark spot on his foot to black paint he had stepped in many years ago. Because the melanoma had gone untreated for so long, the patient would require extensive surgery to remove the cancer that had spread on the bottom of his foot. “If it's found early and small, then you can often remove it, and the overall prognosis is much better,” says Liebman. “The problems that we have, especially in underserved communities, are where people are less educated about the fact that you can get a skin cancer on your foot.”
This lack of awareness, plus a general consensus among patients of color that their pigmentation protects them from most types of skin cancer, means that patients rarely suspect they have skin cancer and therefore often present later. A 2017 article in the British Journal of Dermatology analyzing melanoma survival rates among ALM patients treated at Kaiser Permanente Northern California found little difference by race or ethnicity, but other studies have found lower melanoma-specific survival rates among Hispanic, Asian, and Black populations than in whites. The five-year melanoma-specific survival rate for Blacks is 77.2%, and for Asian/Pacific Islanders, 70.2%, compared with 82.6% survival rates for non-Hispanic whites, according to a 2009 JAMA Dermatology article.
“Combine the fact that there are fewer treatments with a rare tumor that's less studied—it makes for this perfect storm,” says Adewole Adamson, MD, MPP, a dermatologist and assistant professor at Dell Medical School at the University of Texas at Austin. “Black people, when they get it, have worse survival and worse outcomes."
Vito Rebecca grew up thinking he would be an architect after reading Ayn Rand’s The Fountainhead as a boy.
But when he was 14, his mother, who had immigrated to New York from the Dominican Republic, was diagnosed with breast cancer. After what the family thought was a successful course of treatment, the cancer returned, and she passed away when he was 17. He decided to go into biomedical research instead.
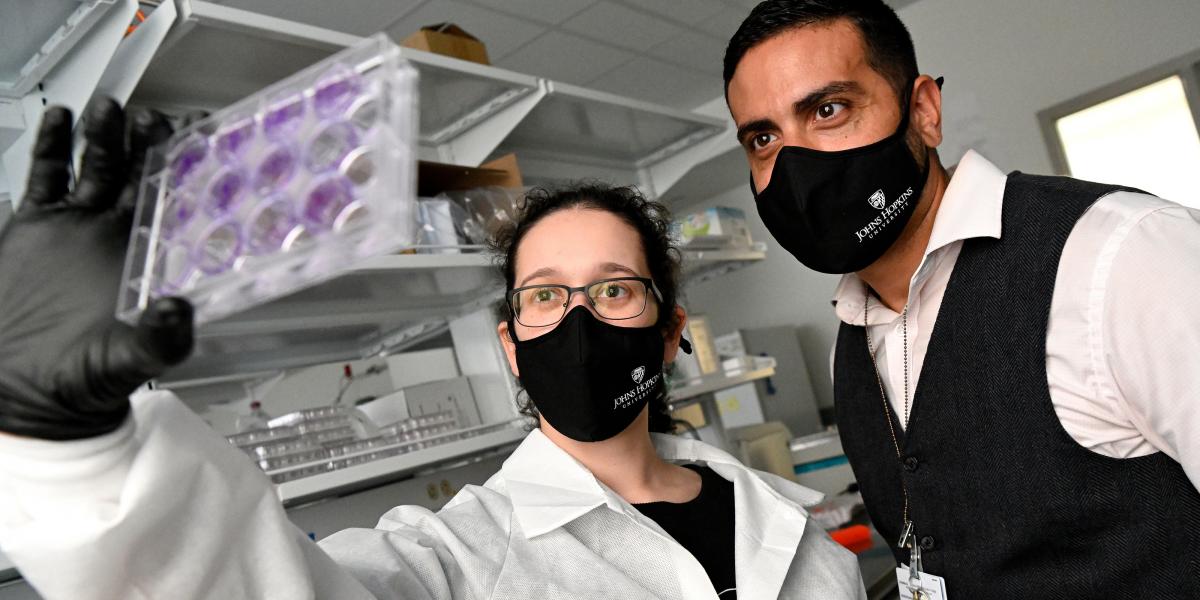
After majoring in biology as an undergraduate and receiving his PhD in cancer biology from the University of South Florida, Rebecca looked around at the cancer research field. “The drivers of acral melanoma remain mysterious,” says Rebecca, now an assistant professor in Biochemistry and Molecular Biology at the Bloomberg School. When he thought about what sort of research to pursue, he had his mother’s cancer recurrence in mind.
Melanoma was an exciting field, but despite the recent breakthroughs in treatments, researchers were still encountering therapy resistance. A common therapy for melanoma, a cocktail of a BRAF inhibitor and an MEK inhibitor (named for the genetic mutations they inhibit), is not available for most patients with ALM due to the unique genetic makeup of ALM cells. Furthermore, there is some evidence that ALM patients are less responsive to immunotherapy overall, though the case numbers of ALM patients are too low to reach conclusive answers.
“No matter what they tried, the [cancerous] cells would come back,” Rebecca says. “It resonated a bit with what my mom went through, and I wanted to begin studying this type of cancer to try to understand resistance, and what it means to try to overcome it with new drugs.”
Rebecca still wears a necklace of his mother’s, a silver-colored chain as a bracelet, looped loosely three times around his wrist. The chain once bore a pendant of St. Peregrine, the patron saint of those with cancer or any incurable disease.
Early on in his efforts to better understand ALM and what makes it so resilient, Rebecca came face to face with a major problem for ALM researchers: the mismatch between the population most affected by ALM and the demographics of the available cell lines with which to study it. Researchers use these cell lines to study either in vitro or by grafting tumor cells onto mice to create what is called a “patient-derived xenograft,” or PDX. There are only 19 ALM cell lines worldwide available today (with a dozen in development) for researchers to study how ALM develops and responds to therapies, says Marc Hurlbert, PhD, chief science officer at the Melanoma Research Alliance. By comparison, five to 10 times as many cell lines are available for more commonly studied cancers such as lung and breast cancers. MRA recently collected the available ALM cell lines in a virtual “catalog” that went live in May. Nearly all of them are from white patients. Just one is from a Black American, one from a Latin American, and one from an Asian patient.
“More work is needed to develop a diverse set of resources to study ALM in the lab,” says Hurlbert.
Rebecca plans to correct this lack of representation by collaborating with dermatologists to collect ALM tumor samples and other types of melanoma samples specifically from patients of color. This will provide a more diverse set of models—cell lines or PDX mice—to study. Rebecca notes that while efforts have been made to increase representation in clinical trials (such as for COVID-19 vaccines), the same effort to diversify has not been widely made in the preclinical setting, where laboratory research takes place before it is tested in humans. “Incorporating a more diverse set of cell lines in the preclinical setting will better ensure that future clinical trials that are based off of preclinical research will more likely benefit patients across all ethnic and racial groups,” Rebecca says.
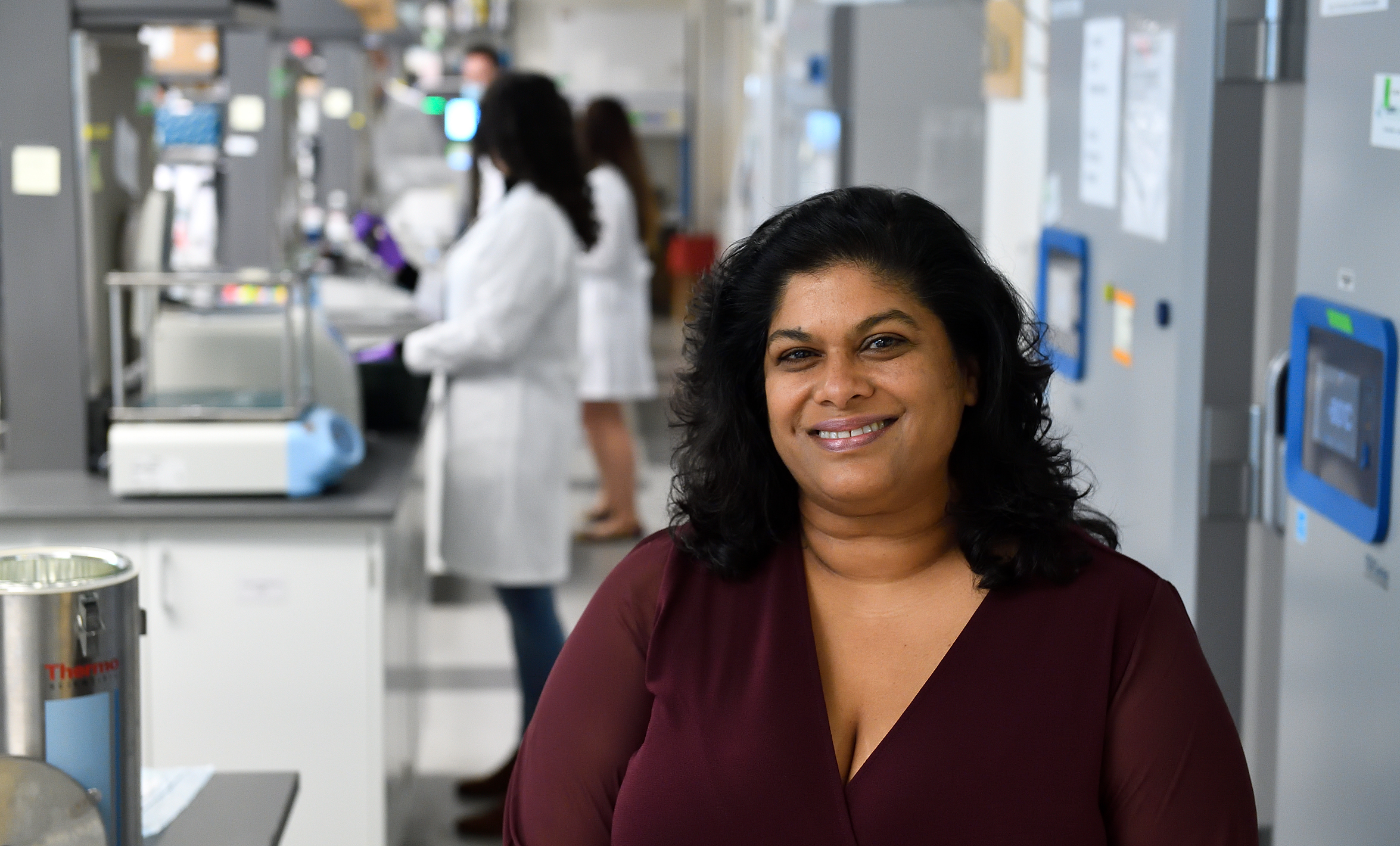
As Ashani Weeraratna, PhD, decides which projects to pursue in her lab, she must weigh the historical neglect of diseases like ALM with other considerations such as the generalizability of research. “It is definitely a balance. What’s affecting most people? What do we need to treat?” asks the E.V. McCollum Professor and Chair in Biochemistry and Molecular Biology at the Bloomberg School. “Acral certainly is a pretty rare disease in general, but I do think the fact that it is so prevalent among communities of color makes it a very important disease to study.”
In Mexico, for example, ALM is the most common melanoma, but there are still relatively few cases overall—perhaps 600–1,000 cases every year, estimates Carla Daniela Robles-Espinoza, PhD, a bioinformatician and assistant professor at the National Autonomous University of Mexico. The National Cancer Institute in Mexico City will typically receive a new ALM patient every week or so. Robles-Espinoza has been working with the Institute since 2018 to collect patient samples from across Mexico; some are sent to a colleague in Brazil to create tumor models or to the UK for genomic sequencing. She and her colleagues also keep some of the samples in-house to create cell lines. Most ALM patients can be treated with excisions or amputations, she notes, but a substantial proportion should receive further treatment to prevent the cancer from spreading to the brain, heart, or liver, for example. “Here in Mexico, patients don't have a lot of options for treatment, because on many occasions, the most recommended therapy would be something like immunotherapy,” says Robles-Espinoza. “But immunotherapy is very, very, very expensive, and it’s not accessible to a lot of people here.” Even in the U.S., the most recently approved crop of immunotherapy drugs can cost hundreds of thousands of dollars a year if the drugs are not covered by insurance.
What makes acral lentiginous melanoma so difficult to treat? In addition to structural and logistical barriers (such as a paucity of models), the lack of insight into its causes, and the historical lag in researching it, ALM is a challenge to study at the molecular and genetic level, too. Melanomas are among the more adaptable types of cancer because it is believed that melanoma cells originate in a type of stem cell called neural crest stem cells. During embryonic development, these stem cells migrate to the skin, eventually differentiating into melanocytes, the cells in our skin that produce the skin pigment melanin. Melanoma can develop when melanocytes mutate. While some drug therapies can effectively target melanoma, Rebecca and other researchers have observed in the lab that melanoma retains a portion of the cancerous cells, regardless of the drug used. These cells appear to survive by reverting into a dormant, de-differentiated state that allows them to escape targeting by the drug and even detection by modern imaging techniques, only to later reemerge with drug resistance.
“This small fraction of tumor cells … they have figured out a way to go away from their melanocyte lineage back to their more ancestral lineage, this neural crest stem cell–like state,” Rebecca explains. “So like a stem cell, they become very adaptable, very plastic, very able to survive all kinds of stresses, be it low oxygen levels, low nutrient levels, or therapy.”
Using this observed commonality between neural crest stem cells and “persister” melanoma cells as a starting point, Rebecca is now investigating what happens at the genetic level that enables these cells to resist treatment. He is doing this by comparing three types of cells: human skin–derived stem cells, melanoma cells, and noncancerous melanocytes. This will enable him to see which genes are expressed in the stem cells and the melanoma cells that behave similarly to stem cells, while the melanocytes will serve as the control cells. “What are those de-differentiated genes that melanoma cells take advantage of to survive? And can we try to target those de-differentiated genes as a new way to kill that small part of the population [of cells] that existing therapy cannot kill?” Rebecca asks.
Another area ripe for further research is what causes ALM. Unlike most melanomas, which are caused by the sun (also called “UV-dependent”), ALM appears on parts of the body that have limited sun exposure. The skin on these areas—whether it’s the thicker skin of the sole of the foot or the palm, or the nail bed—also has a different composition than the skin on the rest of the body. It has an extra layer, known as the stratum lucidum, that contains higher levels of collagen and keratin, two structural proteins that help keep the skin supple by binding to elastin, explains Weeraratna, who studies the interaction between melanoma, skin aging, and tumor microenvironments (the tissues, cells, and other molecules and fluids that surround a given cell or group of cells).
Two years ago, Weeraratna was getting her toenails painted her usual pearlescent color during a pedicure when she spotted a stripe under her toenail and recognized it as possible ALM. She caught it early enough that it was premalignant, but the experience inspired her to learn more about the disease.
One theory holds that ALM lesions are caused by mechanical pressure against the areas where it commonly occurs, such as the repeated stress on the feet from excessive standing or walking, or the rubbing of a shoe onto part of the foot. “It was interesting to me, because one of the things that we study in my lab is how, as you get older, the mechanical stresses that drive tumor progression and tumor invasion can increase,” Weeraratna says. Her research has shown that older and younger patients can respond differently to drug therapies. “An older patient reacts completely differently to a drug that targets a single gene,” she says. “Nothing else should matter, but you have one gene, and one drug, and an older patient will not respond to that therapy, whereas a younger patient will, and all of that has to do with the microenvironmental factors that are governing that response.”
Weeraratna, who was born in Sri Lanka, also notes that ALM’s higher prevalence in communities of color highlights the need for taking a wide range of demographic factors into account: not just age, but ethnic background and gender, for example, citing the effect of hormone signaling on melanoma.
At the genomic level, ALM is also an unusual beast. When researchers try to understand what causes melanomas, they can perform what is called a “mutational signature analysis,” taking large amounts of genomic data and running a statistical analysis on the patterns and kinds of mutations present. Different types of mutations leave different traces: Mutations caused by cigarette smoking or UV exposure, for example, will leave specific clues in the tumor’s DNA. Unlike most melanomas, ALM has very few changes that affect a single point in the DNA structure. Instead, Robles-Espinoza says, ALM tumors might be missing a large chunk of a chromosome, for example, or will show massive changes in the genome. This makes it very difficult to use algorithms and statistical analysis to capture patterns, since they are working with a small data set, and the data they do have do not seem to display regular, consistent patterns that might point to specific causes.
To address the scarcity of data, Robles-Espinoza and colleagues around the world researching melanoma often work together and share data. “The melanoma community is very tight,” she says. She is also a project partner in the Dermatlas Project, an interdisciplinary and international consortium of researchers (including pathologists, geneticists, and computational biologists) who aim to create a “genomic atlas” of skin tumors. “International cooperation is really important, especially when you have such a rare type of cancer,” Robles-Espinoza says. “You need to pull together a lot of researchers from a lot of places to try and figure out what's going on, because we can't really do it on our own.”
Because ALM is so rare, the U.S. Preventive Services Task Force currently does not recommend annual dermatological screenings for it, nor do most dermatologists. “I do not think that Black people should come for routine screening to see their dermatologist every year,” says Adamson, the University of Texas dermatologist. “I don't think that is a good use of resources.” Instead, he recommends patient education and awareness. “Folks should be aware—if there's anything growing, changing, bleeding, et cetera, on their skin, they should see a physician, you know, preferably somebody with skin expertise, just to make sure it's not a cancer.”
Awareness among other care providers, such as primary care physicians or podiatrists, could also play a role. Stephanie Heart, an ALM survivor who lives outside of Philadelphia, had what she thought was a bleeding blister on her toe. She never imagined it might be cancer. Her primary care provider referred her to a podiatrist, who sent a sample for biopsy but told her he thought it was a wart. While she waited for the biopsy results, she tried to freeze it off using a wart removal kit from the drugstore, which hurt more than she could describe. (“Ouch is an understatement,” she says.) She wishes primary care providers, podiatrists, and even pedicurists at nail salons were trained to identify the signs of ALM. “I've been getting pedicures all these years … and not even seeing those thin little lines,” Heart says.
Suzanne Carothers would like to see a quick check—a glance at the hands, feet, and nails—become a standard element of a general health screening. It was just such a glance by Liebman that saved her life. “One thing that is clear is that I'm alive now because of early detection,” Carothers says. “What often happens to Black and brown people, or all people who don't have economic resources, is they don't have access to quality health care for the symptoms that they see, and they get ignored until they have escalated to a state of metastasis. … Why wouldn't that be a part of a routine exam? Everybody doesn't have a dermatologist.”