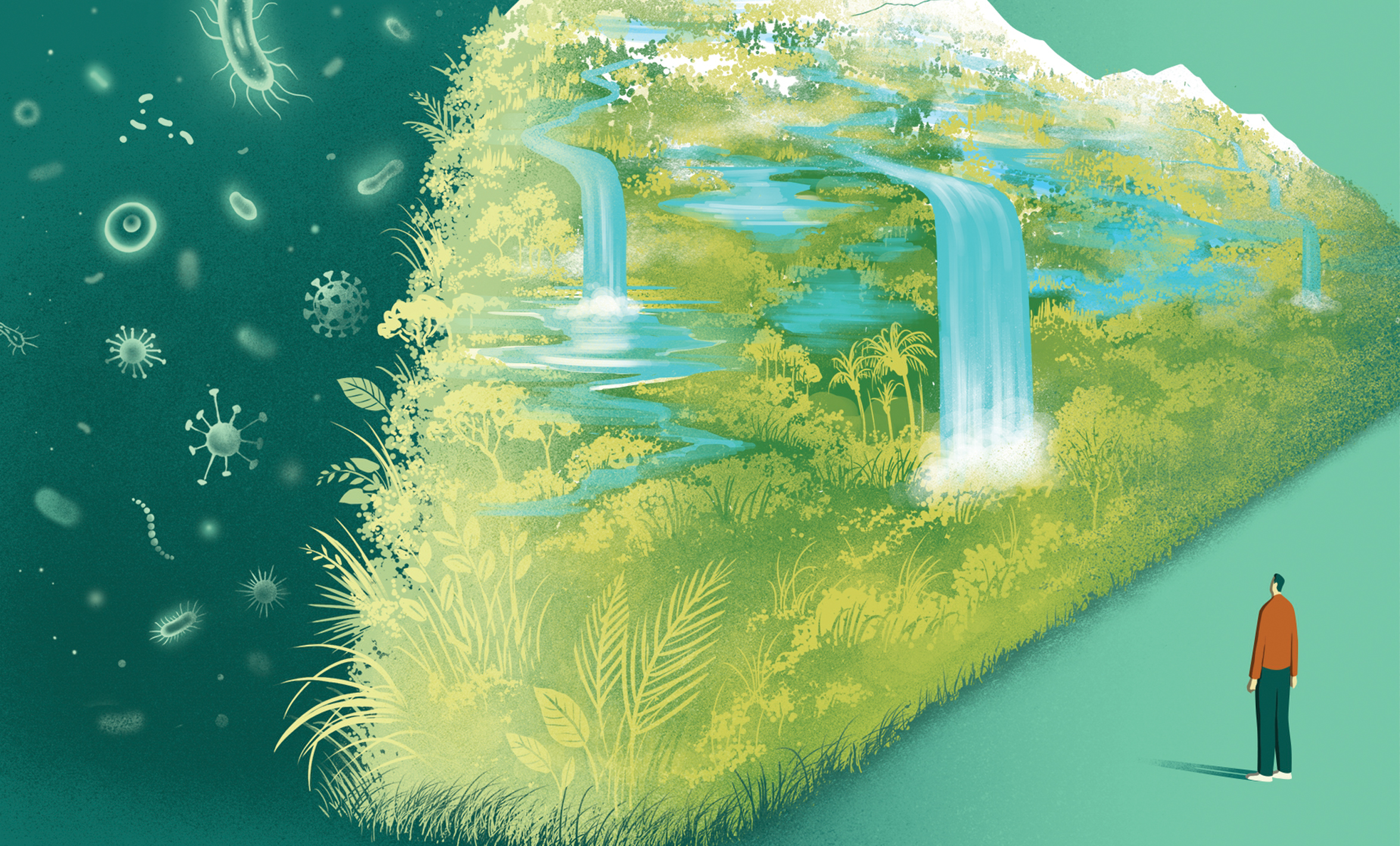
Healthy Ecosystems, Healthy Humans
Biodiversity is one of the best defenses against many infectious diseases.
Cases of mpox are surging. In August, the WHO declared an international emergency due to the dramatic rise in incidence of the disease, which can be fatal to people who are immunocompromised. Since 2022, around 100,000 cases of mpox have been reported, and hundreds of people have died. First detected in a human in the Democratic Republic of Congo in 1970, the virus is now quickly evolving, and mpox strains are spreading rapidly in and beyond Africa.
While human-to-human transmission is now the main driver of the spread, the mpox virus first spilled over to humans from rodents and monkeys, largely because of human-caused changes to the environment. For example, deforestation in West Africa, fueled by logging, brought humans into closer contact with infected animals. Climate change, too, may be extending the breeding season of rodents that carry the virus.
The mpox outbreak is part of an alarming trend. From COVID-19 and Lyme disease to Ebola and dengue fever, every year pathogens carried by animals sicken 2.5 billion people, killing 2.7 million. Over the past century, 60% of all new infectious diseases were the result of animal-to-human spillovers.
And the risk of zoonotic diseases is ballooning. Researchers have estimated that over the next 50 years, more than 15,000 viruses will spill over to a new species—with increased global temperatures and land-use changes driving the increase. Some of these viruses will likely be just a few random mutations away from pandemic potential.
“The problem is big,” says Meghan Davis, an associate professor in Environmental Health and Engineering. “And it’s getting bigger.”
Human activities have directly and indirectly fueled the spread of zoonotic diseases. Long-distance travel, for example, has transported not just people but diseases to new locations. “Think back to the earliest cases of Ebola in the 1970s,” says Davis, DVM, PhD ’12, MPH ’08. “They tended to be in very remote areas, with populations that were geographically cut off. So it would flare up and burn out. But now, people are moving globally all the time—and the risk [of transmission] is that much greater.”
Our decimation of the environment is another cause of the increase. Deforestation means humans can more easily venture into habitats where they might encounter animals that are acting as disease reservoirs, and the destruction of biodiverse areas for large-scale monoculture farms allows pathogens to spread more quickly.
Deforestation in the Amazon basin, which brings human settlements to the edge of the rainforest, increases malaria transmission, with disease risk increasing by 3.3% for every 10% increase in forest clearing. And in sub-Saharan Africa, irrigation schemes, which create standing water, as well as dam construction, have also intensified the malaria threat.
“We have abundant evidence that our destructive use of nature is catching up with us,” says Felicia Keesing, PhD, an ecologist at Bard College. “Zoonotic disease risk is one more reason why we should be reversing course.”
Climate change is a powerful threat driver. As global temperatures rise, disease vectors can spread into regions newly favorable to them. Malaria-carrying mosquitoes, for example, are now showing up in high-altitude parts of Africa, such as the Kenyan highlands, where the frequency and intensity of outbreaks have increased over the past 15 years.
In the U.S., meanwhile, disease-bearing ticks are thriving places they used to find too cold. “Twenty-five years ago, if you didn’t want to get Lyme disease, you could just go to Maine,” says Douglas Norris, a professor in Molecular Microbiology and Immunology. “There were ticks in Maine, but the season was so short that they couldn’t complete their transmission cycle. But now it’s warm enough, and Maine has the highest incidence of Lyme disease in the U.S.”
The warming climate also brings more frequent and more extreme weather events that exacerbate vector-borne disease threats. In July, Hurricane Beryl sparked a surge of West Nile virus in Houston. “The floodwaters created standing water for mosquitoes,” says Norris, PhD, MS, who is a co-principal investigator on a National Science Foundation–supported project in Houston that is developing an enhanced surveillance system for detecting and predicting mosquito-borne diseases like malaria and West Nile. “Now, they’re going to have to spray the bejesus out of the city.”
Not all zoonotic diseases are intensified by recent environmental changes, though. Epidemiologist Emily Gurley, who studies the bat-borne Nipah virus, which has a mortality rate between 40% and 75%, believes that land-use changes likely played a role in creating the context for outbreaks of that virus. But in Bangladesh, “almost all the forests were cleared 300 years ago,” says Gurley, PhD ’12, MPH, distinguished professor of the practice in Epidemiology. And climate change, she says, might actually reduce outbreaks. Nipah outbreaks are driven by humans drinking contaminated date-palm sap, and people drink more of it in colder years. “So as the planet gets warmer,” says Gurley, “then maybe you'll see fewer spillovers” of this virus.
And while Lyme disease is creeping northward, it’s moving south, too. “That’s not consistent with climate change,” says Richard Ostfeld, PhD, a disease ecologist at the Cary Institute of Ecosystem Studies, who has studied Lyme disease with Keesing for many years. In theory, the Southern climate has long been hospitable to the disease-carrying ticks, so “there must be other factors involved as well. And, to a great extent, we don’t know what those other factors are.”
What we do know is that biodiversity is a barrier against disease. Flourishing ecosystems safeguard humans from a panoply of zoonotic illnesses. But as those ecosystems become less diverse—primarily because of habitat loss and fragmentation—that barricade begins to crumble.
Take Lyme disease. “The general hypothesis is that where there is a more diverse array of animals for ticks to feed on, that dilutes the intensity of the pathogen,” says Norris. A greater diversity of species means that pathogens infect many animals, including those least likely to transmit the disease. Ostfeld and Keesing first termed this phenomenon the “dilution effect,” which they documented in forests of the Eastern U.S. “When you lose that biodiversity,” says Keesing, “you lose that protection.”
In such forests, the white-footed mouse has a higher probability of transmitting the Lyme-causing bacterium, as compared with the other animals that ticks feed upon, including squirrels and skunks. In areas with large numbers of white-footed mice in relation to squirrels and skunks, the probability that a tick will attach to a white-footed mouse increases.
Climate change, as a driver of biodiversity loss, is part of the dynamic too. “Climate change is predicted to cause one in six species on the planet to go extinct,” says Jason Rohr, PhD, MA, a professor of ecology and public health at the University of Notre Dame. “And even though we’ve seen a lot of biodiversity loss already, I think we’re only going to see greater amounts of it in the future.”
Along with uncovering the size and the shape of the risk, researchers are addressing the threat. Norris, for his part, has helped develop sophisticated monitoring techniques for detecting the next outbreak of mosquito-borne diseases. Using robotic traps, Norris’ team can identify specific species of mosquitoes, which gives a clue as to which diseases they might be carrying. Then, using genomic analysis, Norris and his team also search for the genetic codes of any new pathogens that the mosquitoes might be carrying.
Some of the problems we create, though, are more intractable. Ostfeld and Keesing recently wrapped up the Tick Project, a five-year study of a community-based model to prevent Lyme disease. A 2016 CDC study had shown that spraying peoples’ yards with pesticides did not reduce tick encounters, so Ostfeld, Keesing, and collaborators distributed almost 10,000 bait boxes, for killing ticks, to 24 different neighborhoods across Dutchess County, New York. They saw a 50% reduction in the number of ticks, but no reduction in the incidence of tickborne diseases—suggesting that more research is needed to understand where and how humans encounter infected ticks.
Above all, says Rohr, we urgently need “to minimize the impact that we have on the natural world.” Reducing carbon emissions and conservation efforts to halt biodiversity loss will help, as will buying local goods since transporting food products across long distances risks introducing pathogens into new areas.
Flourishing, diverse ecosystems are the most effective safeguard against viral spillover, says Rohr. “We need to appreciate the value that the natural world offers to humanity, from an infectious disease-mitigation standpoint.”
