South Sudanese "Lost Boy" to Postdoctoral Fellow in the Center for Humanitarian Health
My life as a Lost Boy gave me the experience and drive to help displaced people around the world.
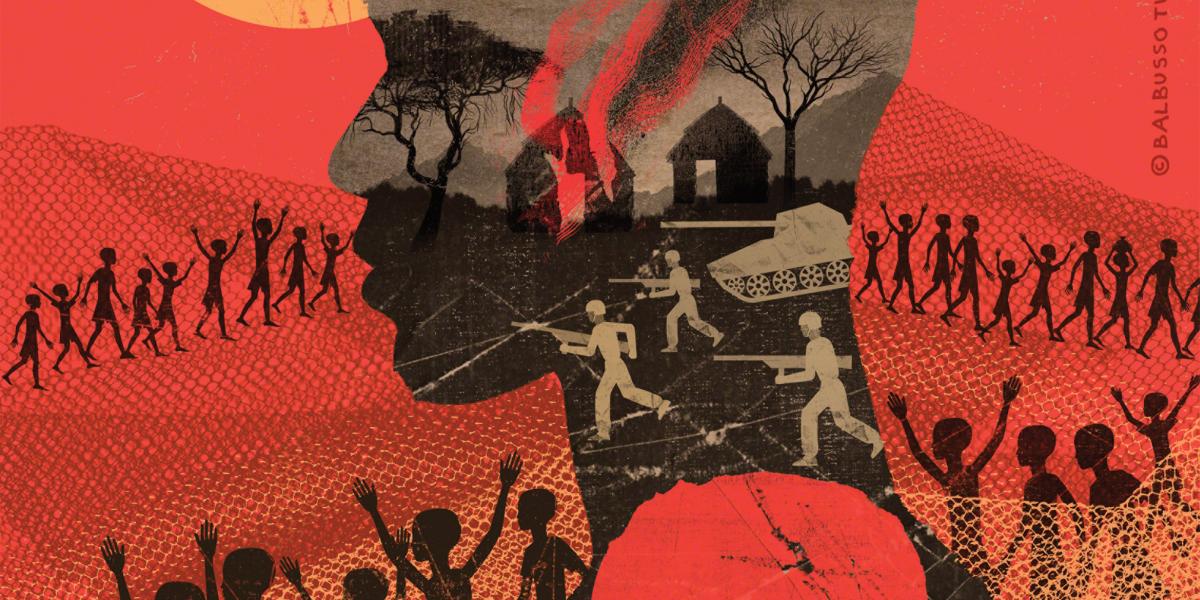
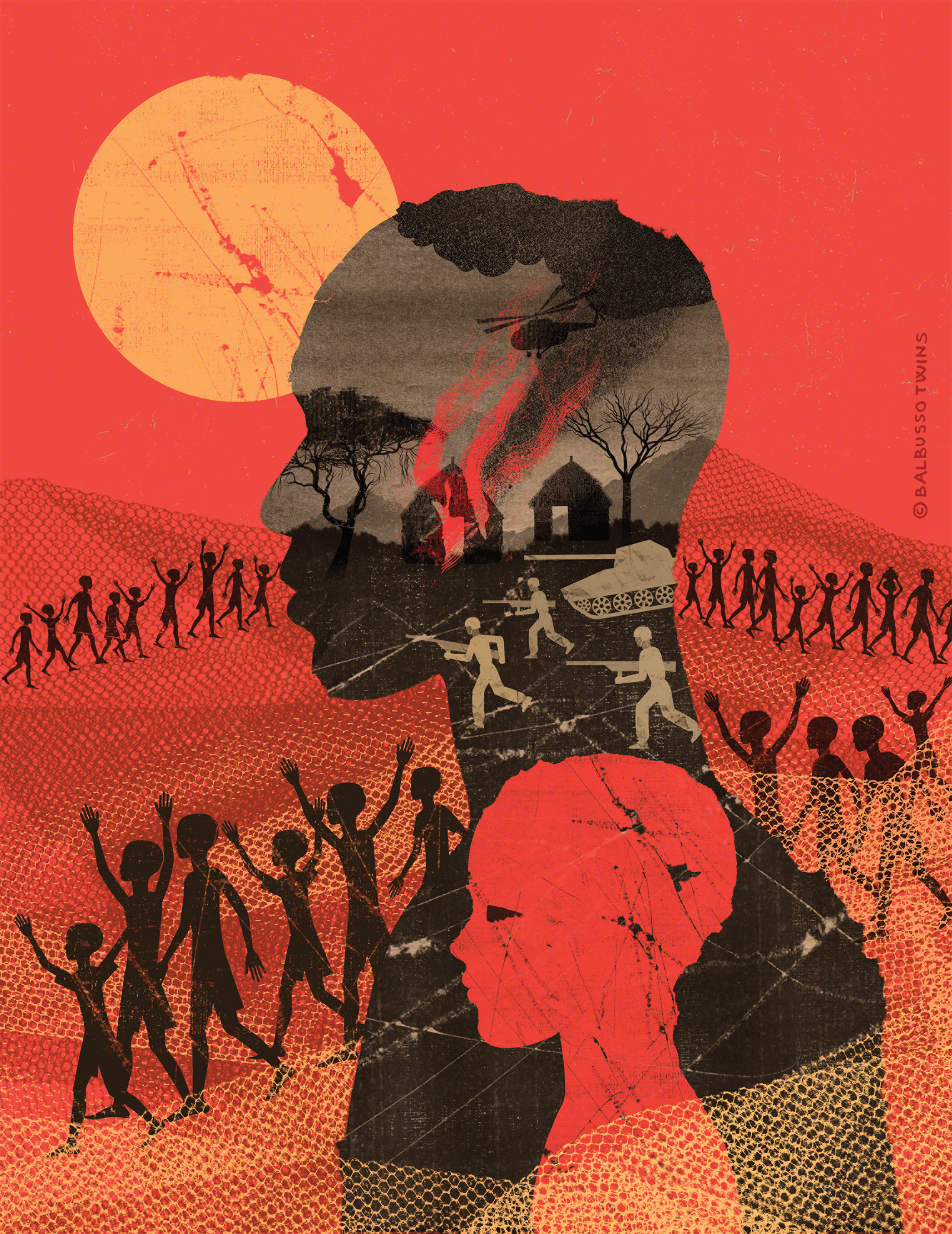
In Maar, South Sudan, my job was to wake up at dawn and take my family’s goats and cows to find grass and water. One morning in 1991, I was caring for the animals when I heard gunfire and screaming. When I ran to see what happened, I saw my village on fire. The rebel forces from Northern Sudan had invaded, and I knew that my family members had either been killed or taken into slavery. I was 6 years old.
Along with other young boys whose villages were destroyed, I started walking.
As we trekked through the wilderness, we endured malnutrition, dehydration, exhaustion and worse. One night when I was hiding in the bush, one of the boys yelled “lion!” I fled—and ran into a sharp branch that cut my leg so deeply I could see bone. There was no way to get medical treatment. Miraculously, it didn’t get infected.
Of the estimated 26,000 to 30,000 children like me who started the journey from South Sudan, about 10,000 died before reaching refugee camps in Kenya. Walking nearly 2,000 miles, I saw many boys die from communicable diseases such as hepatitis B, measles, pertussis and tuberculosis. Like them, I’d had no vaccinations. The refugee camps where we ended up were overcrowded and prone to outbreaks of cholera, shigellosis and other diarrheal diseases, affecting younger children the most.
After nine years at Kakuma Refugee Camp in Kenya, I was resettled in a foster home in Lansing, Michigan. I found myself in a classroom for the first time, as a high school freshman.
I became interested in biology. I majored in it in college, thinking I might someday return to the refugee camps as a doctor. In my senior year of college, with a fellow Lost Boy, I cofounded Southern Sudan Healthcare Organization, which provides health education and health care through a medical clinic. When I sat down with my adviser to figure out my next steps after graduation, he told me about the field of public health. The more I learned, the more I saw this as a way to help the vulnerable populations I left behind in Africa.
I earned my MPH at Michigan State University and then completed my PhD in Environmental and Global Health at the University of Florida. My dissertation was titled “Characterization of Risk Factors, Morbidity, and Mortality Associated with Diarrheal Disease Among Children Under Five (CU5) in East African Refugee Camps.”
Now, as a postdoctoral fellow in the Center for Humanitarian Health, I am serving as a teaching assistant and contributing to research on integrating refugees into national health systems. My perspective as a former refugee is valuable in both of these roles.
I saw firsthand how factors such as refugees’ lack of access to health insurance and health services in their new communities and providers’ lack of cultural competency make it difficult to integrate refugees into the U.S. health care system. Public health professionals can help bridge these gaps. They can create training materials for health care providers. They can partner with resettlement agencies to create health-promotion programs for refugees. They can get—and give—training in the public health issues that affect refugees before they are resettled in the U.S. or elsewhere. In my teaching, I hope to inspire students to join me in this work.
My journey from South Sudan has in some ways taken me back there. I saw and lived the public health problems of refugees on my way to a career in public health. Now I want to be part of the solution. I have been helped in so many ways by others, and to be able to give back—by helping people in the U.S., in Africa and someday around the world—is the greatest gift.
Jacob Atem, PhD, MPH, is a postdoctoral fellow in the Center for Humanitarian Health, which is housed within the Department of International Health.