Public Health Pioneer Henry Mosley on Family Planning, Disasters and Educating Next Generations
In a career spanning decades and continents, Henry Mosley quietly transformed the field of public health.
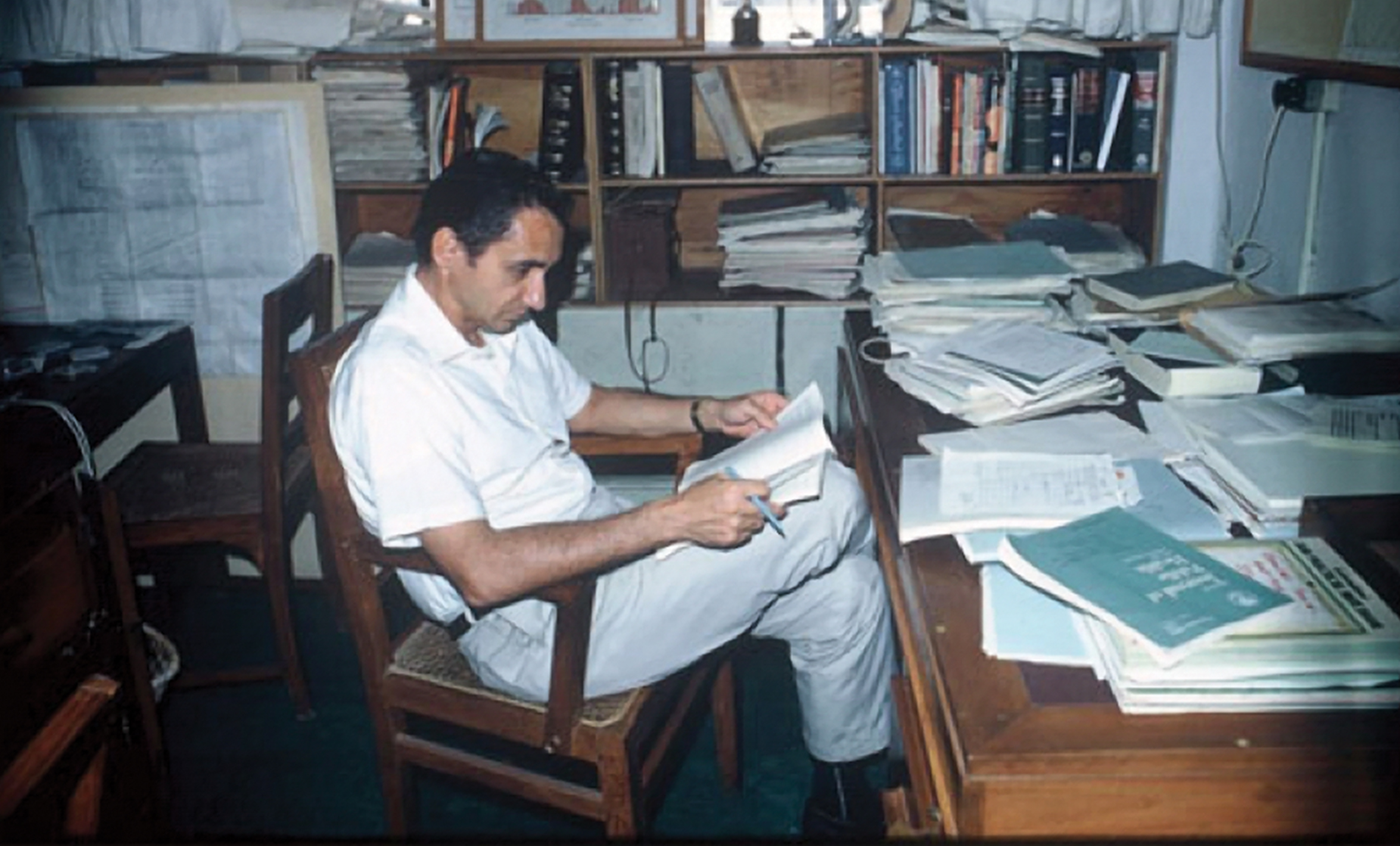
“I like to start new things,” Henry Mosley, MD, MPH ’65, says in his soft southwestern drawl.
It’s a classic understatement from Mosley, now 85 years old and a professor emeritus at the Bloomberg School.
Barely a year after earning his MPH, he was conducting cholera vaccine field trials in Matlab, a densely populated rural area in East Pakistan (now Bangladesh). Many of its hundreds of cholera-prone villages were accessible only by boat or by slogging across acres of rice paddies.
Because only three people out of a thousand in an endemic region typically get cholera each year, the trials required large numbers of cases and controls to achieve statistically significant results. But because the disease kills so quickly, anyone who fell ill had to be treated immediately. At one point, that meant having 1,400 fieldworkers visit 285,000 people in 233 villages—every day.
Alex Langmuir, MPH ’40, founding director of the CDC’s Epidemic Intelligence Service, had appointed Mosley head of the epidemiology unit at the Pakistan-SEATO Cholera Research Laboratory in Dacca (now Dhaka). When he first arrived, the fieldworkers in Matlab were focused exclusively on the signs and symptoms of diarrheal disease. But Mosley saw an opportunity to do more. Inspired by a demography course with biostatistician Helen Abbey, ScD ’51, he reckoned, “Gee, if you’re going to visit every house every day, why just look for cholera?”
Mosley directed the fieldworkers’ supervisor, the Bangladeshi sociologist and anthropologist K.M.A. Aziz, to expand their surveys to include demographic data—births, deaths, marriages, divorces and migrations—as well as questions on contraceptive use.
Mosley’s demographic surveillance system would make Matlab one of the richest sources of longitudinal demographic and health data in the developing world—as well as a testbed for evaluating public health interventions that have influenced health care policy around the globe.
This was only the beginning of a long career as a serial innovator.
Mosley would go on to do pioneering work in disaster epidemiology, family planning and child survival; establish multiple institutions at home and abroad devoted to improving global public health; and launch cutting-edge educational initiatives.
In the process, he changed the nature of public health research, influenced countless public health professionals and helped save millions of lives.
Not that he would ever admit it. If pressed, he will confess that he loves to teach and to build enduring institutions. But self-promotion simply isn’t in his nature.
Instead, he has been content to remain, in the words of School historian Karen Kruse Thomas, PhD, “the man behind the curtain,” boldly seizing opportunity after opportunity to improve the lives of people around the world while somehow managing to draw as little attention to himself as possible.
“Public health was in my blood,” Mosley says.
Despite his twang, Mosley was born in China, where his parents were medical missionaries before WWII.
“My dad saw kids coming in with diarrhea, malnutrition, infections, tetanus,” he says. “And he recognized that public health and preventive medicine were the way to go.”
After earning a doctorate in public health, Mosley’s father served as an epidemiologist in the U.S. Army Medical Corps, taught at universities across the Southwest and worked on family planning programs in India and Turkey.
“I never lived anyplace more than two years until I went to college,” says Mosley, who inherited his father’s wanderlust along with his religious faith and passion for public health. As a devout Christian, Mosley has always seen public health as a moral calling that embodies the values of service, healing and caring for the disadvantaged.
After Mosley earned his MD from University of Oklahoma and completed a residency at Hopkins, he and his wife, Bunny, a nurse, hoped to serve as medical missionaries. But the mission board was looking for surgeons, so Mosley, like many future public health luminaries, joined the EIS and soon found himself posted to Dacca.
Well-funded and located in a country beset by public health challenges, the Cholera Research Laboratory was the ideal setting for a young researcher with plenty of ideas and initiative.
“It’s like a gold mine here,” Mosley wrote to Langmuir in 1966.
Mosley’s field trials, for example, proved that the injectable cholera vaccines available at the time were only 50% effective and lasted for less than six months. Those findings led the WHO to declare that cholera vaccinations should no longer be required of travelers.
Early on, Mosley noticed that the birthrate in Matlab was lower than expected. He discovered that mothers were suppressing ovulation by breastfeeding for 18 months, providing the first evidence of natural birth spacing in a rural population. By allowing researchers to calculate accurate growth curves, the system also revealed that extended breastfeeding without supplementation was causing childhood malnutrition. Because these undernourished children were much more vulnerable to infectious disease, approximately 15% of them died before age 5.
Such findings helped illuminate the complex relationships between reproductive behavior, nutrition and child health. Once Mosley and his colleagues grasped the full extent of the unmet need for contraception in a place where unintended pregnancies were common, they became convinced that better family planning could lower rates of maternal mortality and allow families to devote more resources to the children they chose to have. These changes could foster a social revolution in which women, having gained control of their fertility, would be free to educate themselves and enter the workforce.
“I recognized that family planning was not only good for the health of mother and child, but that it would also transform society,” Mosley says.
“He’s been a real champion of women’s empowerment,” says Saifuddin Ahmed, MBBS, PhD ’96,
a professor in Population, Family and Reproductive Health. Mosley’s work in Matlab so inspired Ahmed that he left his native Bangladesh to study with him. (In the 1990s, they co-authored a study showing that bundling family planning with maternal and child health programs as Mosley did in the 1970s increases uptake of both.)
Implementing family planning programs also jibed with Mosley’s desire to reduce abortion rates—a point he has made in more than one journal article aimed at persuading evangelical Christians to support international family planning efforts. Mosley’s stances on public health sometimes lead to arguments with his co-religionists, particularly when he argues for safe and legal abortion services. But for Mosley, there is no tension between his Christian beliefs and his public health principles.
“I’m a realist,” he says, explaining that he recognizes that abortions are going to occur and should therefore be medically safe. When fellow congregants in his conservative church ask how he can support the practice, he replies, “Well, the alternative is not no abortion; the alternative is unsafe abortion.”
Mosley was just as forthright with the USAID Office of Population when his analysis of the Matlab data showed that Pakistan’s much-celebrated national family planning program, heavily funded by USAID, was failing. The program relied primarily on intrauterine devices, which had uncomfortable side effects and were also out of sync with the country’s conservative Islamic culture. In response, the USAID mission director in Karachi threatened to have Mosley deported if he made his findings public.
Mosley stayed put, however; and in the end, he would have the last word. Ten years after that confrontation, during a second stint in now-independent Bangladesh, he recruited Shushum Bhatia, MBBS, MPH ’74, an OB-GYN who had previously worked with Carl Taylor in the Narangwal Project in India, to design and implement a culturally sensitive, client-centered family planning program. Since young married women who themselves used contraception were best able to convince their peers, the study employed them as community health workers. Rather than pushing a specific contraceptive method, the workers offered women a wide range of options—IUDs, birth control pills, condoms, sterilization—while teaching them about maternal and child health care.
Within two years, more than 30% of couples in Matlab were using contraception and fertility had fallen by 25%.

In 1971, however, the Bangladesh war of independence broke out, marking the end of Mosley’s first tour of duty in the region. Initially, he stayed to help treat the wounded and even did his best to document the atrocities committed by Pakistani forces against Bangladeshi civilians, taking photographs in the countryside and sending them to Senator Edward Kennedy. But in the midst of the crisis, he was offered an opportunity to return to the U.S. with Bunny and their young children to chair the Department of Population Dynamics (now Population, Family and Reproductive Health).
Then as now, the department was distinctly multidisciplinary; and Mosley’s experience combining epidemiology with social science made him the obvious choice as chair to everyone but himself. Even today, he seems surprised to have been hired.
“I was a student in 1965, and in 1971 they asked me to chair a department,” he says with what appears to be genuine bemusement—adding that when one faculty interviewer asked him why he thought he could handle the job, his response was, “I have no idea!”
After six years behind a desk, Mosley got the itch to go abroad again. So when the director of the Cholera Research Lab fell ill and the whole operation was in danger of shutting down for lack of funding, Mosley leapt into the breach, resigning his position as chair and moving back to Dacca in hopes of saving the institution. Over the course of two years, he raised $18 million and negotiated an international charter to establish the International Centre for Diarrhoeal Disease Research, Bangladesh (now the icddr,b)—an organization that has since broadened its scope to tackle problems ranging from domestic violence to childhood malnutrition.
Crisis averted, Mosley spent the next six years working on family planning and child survival in Kenya and Indonesia.
In 1982, UNICEF had launched the so-called “child survival revolution,” a basket of programs that would save the lives of an estimated 12 million children by the end of the decade. But there was a paucity of convincing research in the area. Attempts to explain differing rates of child mortality, for example, typically focused on biological factors while ignoring socioeconomic and cultural ones—or vice versa.
Yet Mosley knew from his work on reproduction that sociologists had merged these medical and socioeconomic models to interpret varying fertility rates. So he and his former Cholera Research Lab colleague Lincoln Chen, MD, MPH ’73, devised a similar framework for analyzing and predicting child survival that took into account both the biological processes that determine child health and mortality (e.g., malnutrition and infection) and the socioeconomic factors that lurk behind them (e.g., poverty and lack of preventive care). Nearly 20 years after its publication in 1984, the resulting paper, “An Analytic Framework for the Study of Child Survival in Developing Countries,” was deemed a public health classic by the WHO for its enduring and pervasive influence on health research.
When Mosley returned to the School to resume his chairmanship in 1985, the digital revolution was just beginning to transform distance education.
“I love teaching, I really do,” he says. “That’s the reason I was interested in distance education, because I just felt like public health education should be more widely available.”
When the CDC advertised funding for developing a certificate-level distance training program for regional public health advisors, Mosley used it to hire instructional designers and software developers to create a full-blown online course.
The success of that initial offering inspired a whole raft of other online courses, culminating in the launch of the world’s first online MPH program in 1999.
The same year, aided by Al Sommer, dean of the School from 1990 to 2005, Mosley and his faculty colleague Laurie Schwab Zabin, PhD ’79, secured funding from the Gates Foundation to establish the Bill & Melinda Gates Institute for Population and Reproductive Health.
At the time, family planning had diminished as a priority for U.S. foreign aid as well as private foundations, jeopardizing much of the progress that Mosley had been instrumental in leading. Today, however, the Institute is currently celebrating 20 years of research collaborations, advocacy initiatives, leadership conferences and global programs aimed at increasing access to family planning and reproductive health care.

Much of the initial Gates Institute grant was spent on a leadership training course that Mosley developed with Benjamin Lozare, director for Training and Capacity Building at the Center for Communication Programs, also based in Mosley’s department.
Their goal was to help public health leaders in developing countries envision, design and implement innovative family planning programs tailored to their own unique circumstances. What began as two-week problem-solving seminars on campus soon grew into onsite training in more than 24 countries. Mosley and Lozare are still teaching the course, which has been adapted to create localized versions at universities from Southeast Asia to southern Africa.
Indeed, Mosley has been such a successful researcher and administrator that it’s easy to overlook his influence as a mentor—unless, of course, you’ve experienced it firsthand.
“He’s the best teacher I’ve ever seen,” says Ahmed. “Sometimes, when I teach, I see Henry in front of me.”
And he exhorts them to start new things and go, as Lozare says, “to places where there are no maps”—to do, in other words, what Mosley himself has done for more than 50 years.
-
1933
Born in China, where his family lived until 1937
-
1959
Earns an MD from University of Oklahoma and begins training at Johns Hopkins Hospital
-
1965
Earns an MPH at Hopkins and is appointed head of the Epidemiology Section, Pakistan-SEATO Cholera Research Lab
-
1970
Receives U.S. Public Health Service Meritorious Service Medal for his leadership in establishing the Matlab Health and Demographic Surveillance System
-
1971
Appointed chair of Population Dynamics and founds the Johns Hopkins Population Center
-
1975
Sent by U.S. Senate to the Middle East to study world health, hunger and the refugee problem
-
1979
Directs and leads the reorganization of the Cholera Research Lab as the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b)
-
1984
With Lincoln Chen, edits a special issue of Population and Development Review on strategies for child survival research that establishes the field’s analytical framework
-
1985
Returns as chair of Population Dynamics and founding director of the Institute of International Programs
-
1989
Advises Nigerian Ministry of Health on developing its national family planning program
-
1990s
Adviser to USAID on strategies for integrating family planning with maternal and child health programs
-
1993
Technical adviser for the World Bank’s 1993 World Development Report and codirector of the section on Disease Control Priorities in Developing Countries
-
1999
With Laurie Schwab Zabin, founds the Bill & Melinda Gates Institute for Population and Reproductive Health at the Bloomberg School
